Advanced Microsurgical Periodontics: Microsurgical Root Coverage, MIST, and the Pinhole Surgical Technique
Why microsurgery matters in modern periodontics
As periodontal care has evolved, the emphasis has shifted from merely eliminating disease to restoring function, minimizing trauma, and achieving predictable aesthetic results. Advanced microsurgical periodontics uses operating microscopes, microsurgical instruments, fine sutures, and refined techniques to treat delicate soft tissues and root surfaces with minimal trauma. The outcomes are often superior to traditional methods: faster healing, less discomfort, better aesthetics, and higher rates of root coverage and tissue stability.
For patients in Islamabad and beyond, these techniques provide durable solutions for recession, sensitivity, and compromised gum architecture without the bulkier incisions and longer recoveries of older approaches. At Tooth Crew Clinic Islamabad, we integrate microsurgical approaches into our periodontal practice to maximize both clinical success and patient comfort.
This guide explains three cornerstone microsurgical approaches:
- micro-surgical root coverage,
- minimally invasive periodontal surgery (MIST), and
- the pinhole surgical technique (PST) for recession correction.
What is micro-surgical periodontics?
Micro-surgical periodontics applies microsurgery principles—magnification, specialized instruments, gentle tissue handling, and micro-sutures—to periodontal operations. The goal is the same as conventional periodontal surgery (disease control, regeneration, aesthetic correction), but microsurgery modifies how the operator reaches that goal:
- magnification (surgical loupes or operating microscope) improves visualization of tissue layers and suture placement,
- micro-instruments reduce trauma and permit smaller incisions,
- ultra-fine sutures reduce scarring and improve coaptation (edge-to-edge tissue contact),
- minimally invasive flap designs preserve blood supply and soft-tissue architecture.
Compared with conventional periodontal surgery, microsurgical techniques typically produce less post-operative pain, faster vascular recovery, improved aesthetic blending, and higher rates of complete root coverage in root coverage procedures.
Why patients prefer it: better-looking, faster-healing gums with lower morbidity and often fewer follow-up adjustments. Why clinicians adopt it: reproducible, more predictable outcomes—especially important in the smile zone.
Micro-surgical root coverage — advanced solutions for gum recession
Understanding root recession and its impact
Gum recession is the apical migration of the gingival margin relative to the tooth crown. It exposes root surfaces, increases sensitivity, promotes root caries, compromises aesthetics, and can gradually weaken tooth support. Causes are multifactorial: traumatic toothbrushing, periodontitis, thin biotype, orthodontic movement, frenal pull, and occlusal trauma.
Root coverage aims to cover the exposed root surface with healthy keratinized tissue. Microsurgical root coverage uses refined techniques to maximize predictable, stable coverage with improved cosmetic blending.
Indications for micro-surgical root coverage
Patients who typically benefit include:
- those with localized Miller class I or II recession defects (front teeth or premolars),
- patients with root sensitivity interfering with diet or quality of life,
- individuals seeking improved aesthetics in the anterior smile zone,
- candidates for restorative treatment that require adequate attached gingiva.
Patient selection is central: ideal cases have good oral hygiene, non-smokers, controlled systemic health, and realistic expectations.
Micro-surgical techniques for root coverage
Several techniques can be adapted to a microsurgical approach; three common ones include:
- connective tissue graft (CTG) with coronally advanced flap (CAF) under magnification
- tunneling technique with a subepithelial connective tissue graft (tunnel + CTG)
- enamel matrix derivative (EMD) or platelet-rich fibrin (PRF) adjuncts with minimally invasive flap design
Microsurgery optimizes each technique by using smaller, precise incisions, atraumatic flap elevation, and micro-sutures that allow perfect tissue edge alignment without tension.
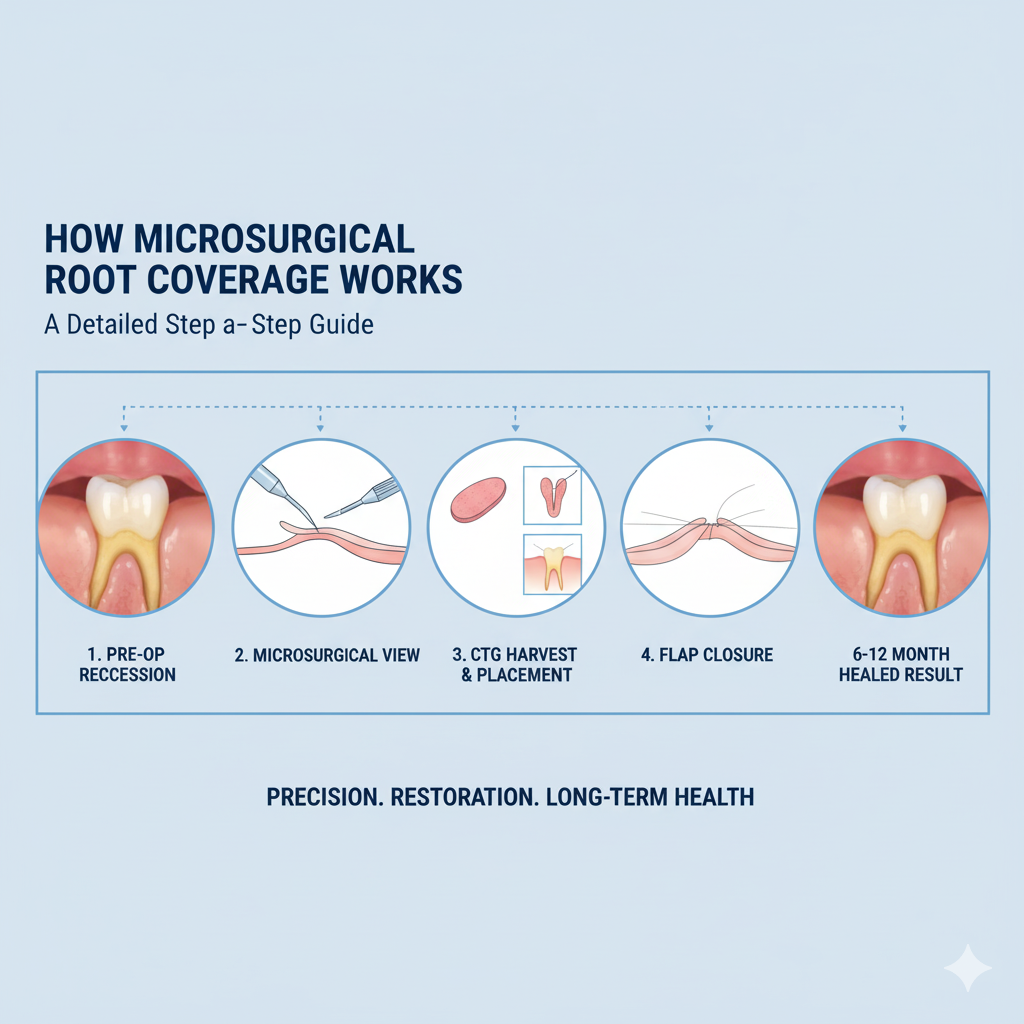
Step-by-step: micro-surgical connective tissue graft with coronally advanced flap (example)
- comprehensive evaluation and photographic documentation
- root preparation: gentle scaling and root planing, chemical root conditioning if indicated (e.g., EDTA)
- local anesthesia with care to avoid excessive tissue distortion
- precise incision design under magnification—intrasulcular or slightly submarginal, preserving papillae
- partial thickness flap elevation using micro-blades and microsurgical elevators to create a tension-free flap
- harvesting of a thin connective tissue graft from the palate using a micro-harvesting technique (single incision or trap-door) to reduce donor site morbidity
- graft placement and stabilization in the recipient tunnel or bed; micro-sutures ensure graft immobility and intimate contact with the root surface
- coronally advance flap margin to fully cover the graft and suture with ultra-fine monofilament (6-0 to 8-0) for precise edge adaptation
- protective dressing if needed; immediate post-op instructions and analgesia
Outcomes and evidence
Microsurgical root coverage demonstrates higher rates of complete root coverage and better color/texture blending compared to conventional approaches in numerous clinical studies. When combined with connective tissue grafts, predictable coverage of single and multiple recession defects is routinely achieved. The stability of the result depends on controlling etiologic factors (e.g., changing brushing habits) and maintaining plaque control.
Benefits for patients
- superior esthetic outcomes (smooth gingival margins and color match)
- decreased postoperative pain and swelling
- faster soft-tissue integration and less scarring
- higher probability of full root coverage in properly selected cases
Risks and limitations
- donor site morbidity (though reduced with micro-harvesting techniques)
- incomplete coverage in very advanced defects or unfavorable anatomy
- technique-sensitive—requires experienced microsurgical clinicians and specialized equipment
- smoking and uncontrolled systemic disease reduce success rates
Cost considerations (Indicative, Islamabad-focused)
| Procedure type | Typical Islamabad range (PKR) | Notes |
| Microsurgical connective tissue graft + CAF (single tooth) | 40,000 – 90,000 | Depends on complexity, number of teeth |
| Tunneling + CTG (multiple adjacent recessions) | 70,000 – 160,000 | Economies of scale for multiple sites |
| Adjuncts (PRF / EMD) | 8,000 – 25,000 extra | Improves healing/regeneration in selected cases |
Minimally Invasive Periodontal Surgery (MIST)
Concept and rationale
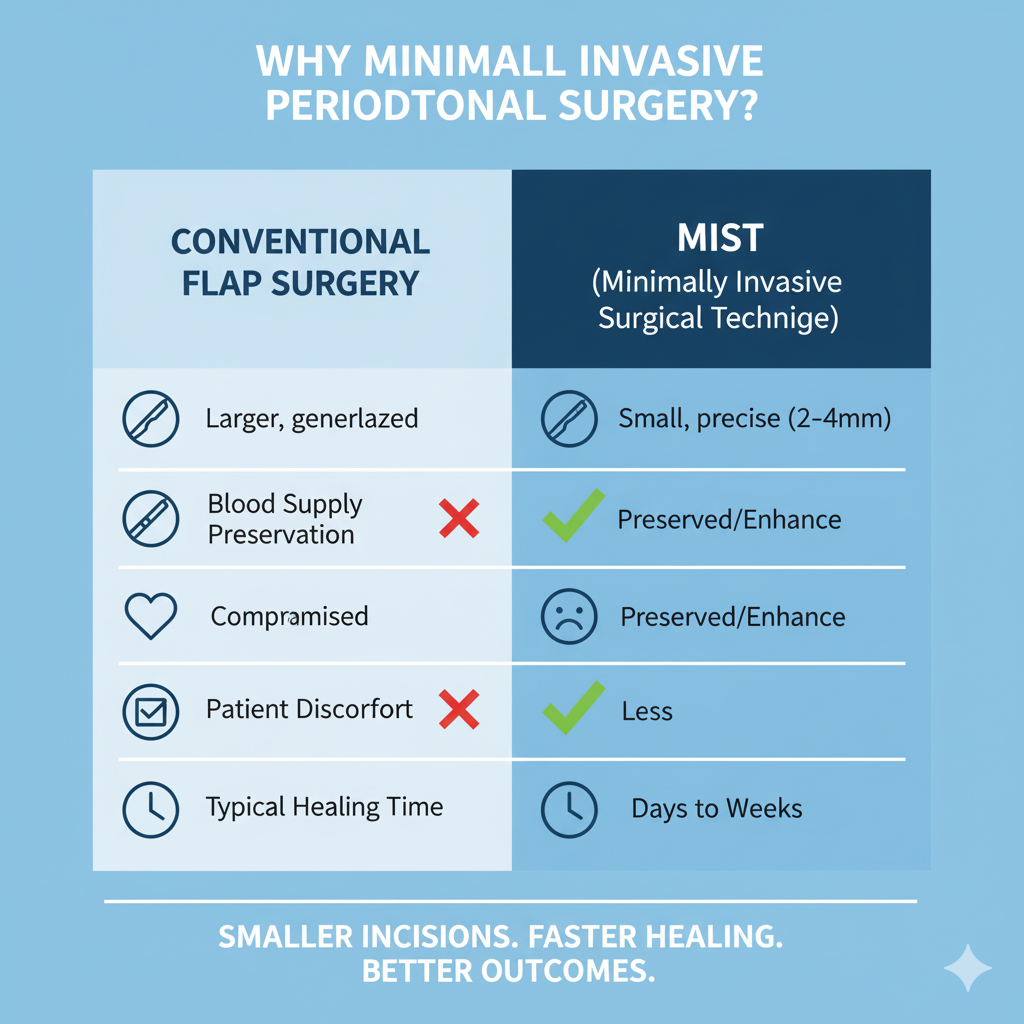
MIST (minimally invasive surgical technique) was developed to treat periodontal defects with the least amount of tissue manipulation required to achieve regenerative outcomes. The core principles are minimal flap elevation, preservation of blood supply, limited incision size, and precise debridement. MIST is often used for intrabony defects and combined with regenerative materials or biologics to enhance bone and attachment regeneration.
MIST can be performed with microsurgical tools and magnification, and is philosophically aligned with modern medicine’s shift towards minimal invasiveness.
Indications for MIST
- isolated intrabony defects amenable to regenerative therapy
- interdental defects where soft tissue preservation improves outcomes
- patients desiring reduced postoperative morbidity and faster return to normal function
MIST procedural overview
- diagnosis with clinical probing and CBCT imaging to assess defect morphology
- small papilla-preserving incisions to access the defect without widening the interdental space
- meticulous debridement of root surfaces and defect using micro-curettes and ultrasonic tips
- placement of bone grafts, membranes, or biologic agents (e.g., EMD, PRF) as indicated
- tension-free closure of soft tissues with micro-sutures to maintain a sealed environment for regeneration
MIST strategies include variants like SUPRA (supra-alveolar papilla preservation), papilla preservation flap, and modified papilla preservation techniques (MPPT) which are selected according to defect anatomy.
Advantages and clinical outcomes
Clinical studies have shown MIST produces favorable outcomes in terms of pocket reduction, gain in clinical attachment level, and bone fill—often with less postoperative discomfort and faster healing than conventional open-flap procedures. Preservation of papillae is particularly important for aesthetic zones.
Practical tips for clinicians
- use microsurgical instruments and magnification to maintain delicate tissue edges
- choose graft and biologic materials based on defect architecture (one-wall vs. two/three-wall defects)
- ensure primary closure — soft tissue sealing is critical for regenerative success
Cost and resource implications
MIST tends to require specialized instruments and clinician training which can raise costs slightly, but faster recovery and improved outcomes often justify the investment for both clinic and patient.
Pinhole Surgical Technique (PST) for recession correction
What is the pinhole surgical technique?
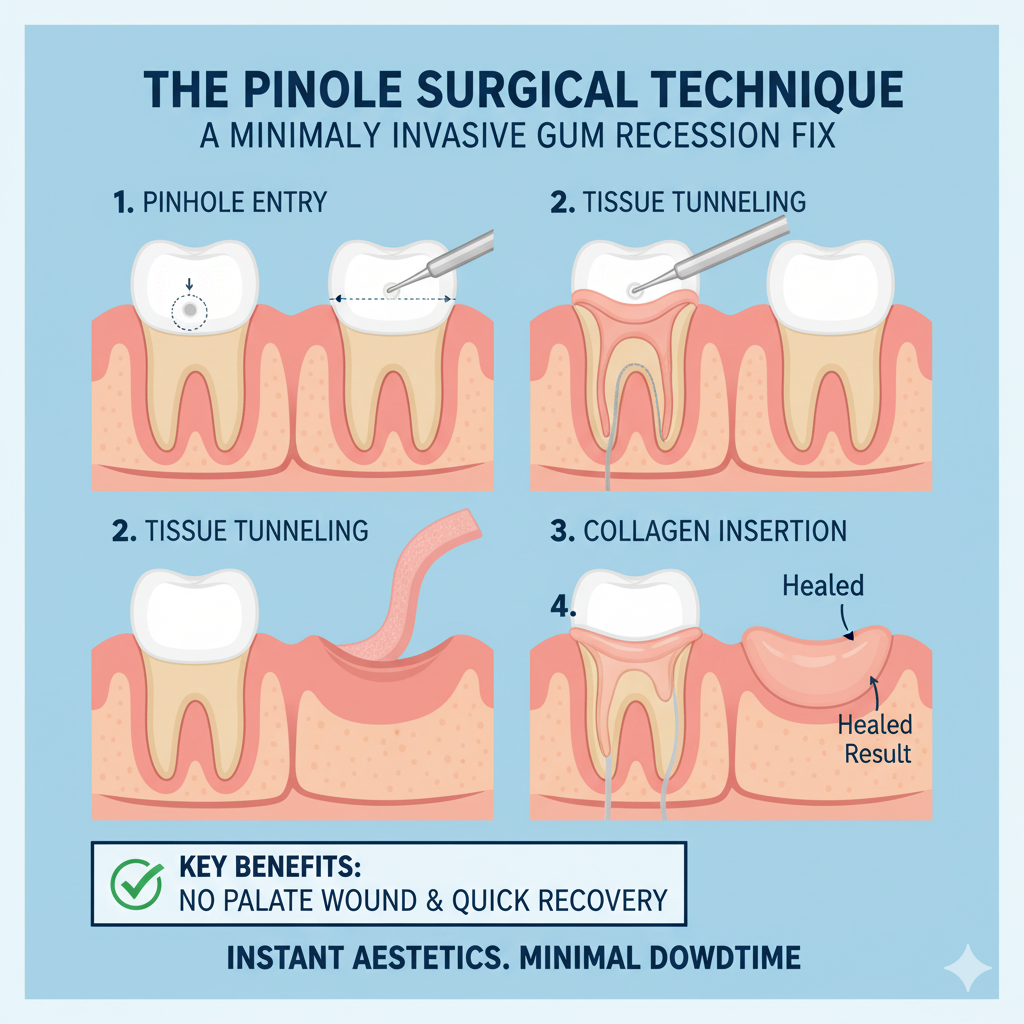
The pinhole surgical technique is a minimally invasive, sutureless method to treat multiple adjacent recessions. Instead of harvesting graft tissue from the palate, PST uses a small (2–3 mm) ‘pinhole’ incision in the mucosa above the recession sites. Specialized instruments gently release the tissue and advance it coronally over the exposed roots. Collagen strips or other graft substitutes are often inserted beneath the repositioned tissue to provide volume and stabilization.
PST is particularly appealing to patients because it avoids a palatal donor site and tends to have minimal bleeding and quick recovery.
Indications and limitations
PST is ideal for:
- multiple adjacent recessions in the aesthetic zone,
- patients who prefer to avoid a secondary donor-site procedure,
- shallow to moderate recession defects with adequate tissue mobility.
Limitations:
- extreme or very deep recession defects may still require connective tissue grafting,
- technique-sensitive, requires clinician training and correct instrumentation,
- long-term comparative data vs CTG are still developing though short-to-medium term results are promising.
PST procedural steps (typical)
- local anesthesia with careful injection technique
- creation of a small pinhole incision in the alveolar mucosa above the defect
- gentle subperiosteal tunneling and release of tissues using specialized PST tools
- coronal repositioning of the soft tissue over the root surfaces
- insertion of collagen strips or resorbable matrices beneath the repositioned tissue to maintain elevation
- supportive dressing and post-operative instructions; no sutures required
Outcomes and evidence
Early and mid-term studies of PST report high rates of root coverage and patient satisfaction, especially for multiple adjacent recessions. Outcomes are improved further when combined with bioactive materials (PRF, collagen matrices) that support tissue integration.
Advantages for patients
- one surgical site (no palate donor)
- reduced operative time and postoperative discomfort
- rapid recovery and minimal visible scarring
- excellent cosmetic blending when performed by experienced clinicians
Risks and considerations
- potential for partial root coverage in complex defects
- careful case selection is essential for predictable outcomes
- operator-dependent — learning curve exists
Cost indications
| Procedure | Islamabad range (PKR) | Notes |
| Pinhole surgical technique (multiple teeth, anterior segment) | 60,000 – 150,000 | Price varies with number of teeth treated |
| PST with collagen matrix | 75,000 – 180,000 | Adds material cost |
Comparative Overview of Microsurgical Approaches
Choosing between microsurgical root coverage, minimally invasive periodontal surgery (MIST), and the pinhole surgical technique (PST) depends on the clinical scenario. Below is a comparative framework.
| Feature | Microsurgical Root Coverage (CTG + CAF / Tunnel) | MIST (Minimally Invasive Periodontal Surgery) | Pinhole Surgical Technique (PST) |
| Main Goal | Cover exposed roots, increase keratinized tissue | Regenerate periodontal support in intrabony defects | Correct multiple recession defects without graft harvesting |
| Surgical Access | Small flap, micro-sutures, graft required | Small papilla-preserving incisions | Pinhole access in mucosa |
| Donor Site Required? | Yes (palate graft unless biomaterials used) | No | No |
| Healing | 2–3 weeks, donor site discomfort possible | 1–2 weeks, minimal pain | 1 week, very rapid healing |
| Esthetic Outcomes | Excellent blending, especially with tunnel techniques | Not primarily esthetic (functional regeneration focus) | Excellent, no visible scars |
| Predictability | Very high when anatomy favorable | High for pocket reduction and regeneration | Good for mild-moderate recession; long-term data still evolving |
| Cost (Islamabad) | 40k–160k PKR depending on teeth | 60k–150k PKR | 60k–180k PKR |
Patient Selection & Pre-Operative Optimization
Before any microsurgical periodontal procedure, thorough assessment is essential.
Medical considerations
- Diabetes: acceptable if HbA1c under control (<7%).
- Hypertension & cardiac patients: ensure stable control, sometimes require medical clearance.
- Anticoagulants: often continued, but surgeon may adjust depending on INR.
- Smoking: dramatically reduces success — patients should quit at least 2 weeks before and 6 weeks after surgery.
Periodontal stability
- Active gingivitis or periodontitis must be treated first.
- Patients should demonstrate good plaque control (O’Leary index <20%) before surgery.
Behavioral factors
- Soft-bristle toothbrushing and atraumatic technique must be taught pre-op.
- Commitment to follow-up is non-negotiable.
Recovery & Aftercare Protocols
Different microsurgical procedures have slightly different post-op protocols, but general guidelines include:
- First 48 hours
- Cold compresses intermittently to reduce swelling.
- Avoid brushing the surgical area; use chlorhexidine rinse if prescribed.
- Stick to soft diet: soups, yogurt, boiled vegetables.
- First week
- No smoking, alcohol, or vigorous exercise.
- Continue gentle hygiene in non-operated areas.
- Pain typically controlled with NSAIDs; opioids rarely needed.
- Suture removal (if used)
- Usually 7–10 days post-op for microsurgical sutures.
- 2–4 weeks
- Gradual return to normal diet.
- Gently brush surgical area with ultra-soft brush when approved.
- Long-term
- Professional cleaning every 3–6 months.
- Monitoring of tissue stability with photographs and probing.
Evidence and Success Rates
Microsurgical root coverage
- Studies report 70–90% complete root coverage with CTG + CAF under microsurgical approach.
- Aesthetic integration scores (color match, tissue blend) are consistently higher than conventional surgery.
Minimally invasive periodontal surgery (MIST)
- Clinical trials show 2–4 mm mean clinical attachment gain and significant bone fill in intrabony defects.
- Patients report less pain and swelling vs. traditional open-flap surgery.
Pinhole surgical technique (PST)
- Short- to mid-term studies (1–5 years) show 80–90% root coverage for mild-moderate recession.
- High patient satisfaction due to quick recovery and absence of donor site.
- Longer-term comparative data still needed vs. CTG gold standard.
Mini Case Examples
Case 1 — Microsurgical Root Coverage
Patient: 28-year-old female, Miller Class I recession on upper canines.
Treatment: CTG harvested with single-incision technique + CAF under magnification.
Result: 100% root coverage at 12 months, improved keratinized tissue width, no donor site complications.
Case 2 — MIST with bone graft
Patient: 45-year-old male, intrabony defect on lower molar.
Treatment: MIST with papilla preservation + demineralized bone allograft + EMD.
Result: 3 mm pocket reduction, radiographic bone fill, minimal postoperative discomfort.
Case 3 — Pinhole Technique
Patient: 34-year-old female, multiple adjacent recessions upper premolars and canines.
Treatment: Single pinhole access + collagen strips.
Result: Esthetic root coverage achieved across 6 teeth, patient back to work next day.
FAQs
- How long do microsurgical periodontal procedures last?
When properly indicated and maintained with good oral hygiene, results can last 10+ years. Root coverage stability is highest in non-smokers with thick biotype. - Which is better: pinhole technique or connective tissue graft?
CTG remains the gold standard for predictability, especially in deep recession defects. PST is an excellent alternative for patients seeking minimal invasiveness and faster recovery in moderate cases. - Is microsurgical periodontal surgery painful?
No — anesthesia prevents intraoperative pain, and postoperative discomfort is mild compared to traditional surgery. Many patients resume daily routines within 24–48 hours. - Can these procedures be combined with cosmetic dentistry?
Yes. Gum microsurgery often precedes veneers, crowns, or orthodontics to ensure stable gum margins and improved esthetics. - How do I know if I need microsurgical root coverage?
If your gums are receding, your teeth appear longer, or you feel sensitivity near the gum line, you may be a candidate. Consultation with a periodontist can confirm suitability. - What’s the difference between MIST and traditional flap surgery?
MIST uses smaller incisions, preserves tissue, and offers faster healing. Traditional flap surgery provides access but often with more morbidity.
Why Tooth Crew Clinic Islamabad is the best choice
- Advanced technology: surgical microscopes, micro-instruments, and laser adjuncts.
- Specialist care: board-certified periodontists trained in Europe and North America.
- Comprehensive options: CTG, tunneling, MIST, PST, bone and biomaterial integration.
- Affordable excellence: procedures at a fraction of international costs while maintaining global standards.
- Patient-focused: tailored aftercare, comfort-focused protocols, bilingual communication.
Conclusion
Advanced microsurgical periodontics represents the cutting edge of gum surgery. With techniques like microsurgical root coverage, MIST, and the pinhole surgical technique, patients can achieve healthier gums, enhanced aesthetics, and faster recovery compared to conventional methods.
At Tooth Crew Clinic Islamabad, we are proud to offer these advanced treatments at international standards while ensuring affordability for our community. If you are struggling with gum recession, sensitivity, or periodontal disease, a consultation can determine the best microsurgical approach tailored to your needs.